-
Courses

Courses
Choosing a course is one of the most important decisions you'll ever make! View our courses and see what our students and lecturers have to say about the courses you are interested in at the links below.
-
University Life

University Life
Each year more than 4,000 choose University of Galway as their University of choice. Find out what life at University of Galway is all about here.
-
About University of Galway

About University of Galway
Since 1845, University of Galway has been sharing the highest quality teaching and research with Ireland and the world. Find out what makes our University so special – from our distinguished history to the latest news and campus developments.
-
Colleges & Schools

Colleges & Schools
University of Galway has earned international recognition as a research-led university with a commitment to top quality teaching across a range of key areas of expertise.
-
Research & Innovation

Research & Innovation
University of Galway’s vibrant research community take on some of the most pressing challenges of our times.
-
Business & Industry

Guiding Breakthrough Research at University of Galway
We explore and facilitate commercial opportunities for the research community at University of Galway, as well as facilitating industry partnership.
-
Alumni & Friends

Alumni & Friends
There are 128,000 University of Galway alumni worldwide. Stay connected to your alumni community! Join our social networks and update your details online.
-
Community Engagement

Community Engagement
At University of Galway, we believe that the best learning takes place when you apply what you learn in a real world context. That's why many of our courses include work placements or community projects.
About PSYcHE
Background
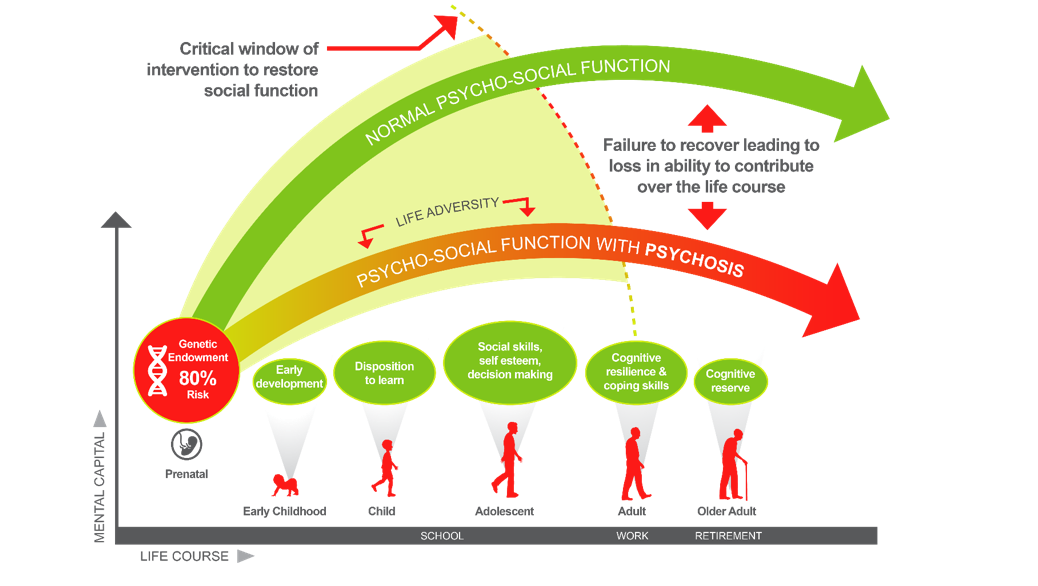
The Government's framework for improved health and wellbeing 2013-2025 (Healthy Ireland, 2013) defines mental health in terms of successfully realising one’s abilities, coping with stress, working productively, and making a contribution to society. It describes the absence of mental health as not just a health issue but also a social and economic issue that will affect 1 in 4 individuals during their lifetime (WHO 2001/2003).
Youth mental health disorders are a major cause of disability nationally and internationally (WHO, 2008) with serious mental health disorders (including schizophrenia and other psychotic disorders) ranked among the top five causes of years lived with disability. Emerging epidemiological evidence indicates that mental ill-health contributes 45% of the burden of disability in those aged between 10 and 25 years. Furthermore, 75% of all mental health disorders first occur between 15-25 years of age and subsequently impacts the most productive years of life. Each year in Ireland an estimated 1,500 people develop a psychotic disorder for the first time. Young people have the poorest access to mental health care of all age groups across the lifespan (McGorry et al., 2013).
Psychosis, even its early stages, can lead to reduced social supports, reduced resilience to stress, and is compounded by other factors. A large emphasis in treatment methods has been placed on targeting the more positive symptoms of psychosis (e.g. delusions, hallucinations etc.), with the assumption being that this would lead to improved functional outcomes. While the positive symptoms are attenuated, the same cannot be said for negative symptoms (e.g. impairments in cognitive functioning, social functioning etc.) For a person to move towards the best recovery possible, it has become increasingly apparent that interventions targeting positive symptoms alone are not enough. More recent research is showing that in order to improve functional outcomes, more attention must be placed on psycho-social interventions targeting social recovery. It is the theoretical underpinning of this project to explore how this can be predicted, achieved, and implemented.
More about the PSYcHE Programme

PSYcHE will target two groups:
-Those with continuing low levels of psychosocial function, even after receiving current best practice interventions.
-Those with higher levels of function following early intervention to determine how best to help maintain the benefits already achieved using online clinician moderated supports.
Our main objectives with both groups will be to establish the feasibility and acceptability of the interventions trialled.
Our vision is to:
1. Build knowledge
Identify predictors associated with social recovery and psychosocial interventions.
2. Establish clinical academic partnerships
Establish Irish/International consortium for Early Intervention for Psychosis (EIP) Services.
3. Translate knowledge into practice
Influence current policy through collaboration with the National Clinical Program for EIP.
Develop evidence base to inform international guidelines.
4. Build Capacity
Introduce a national training hub for psychosocial interventions.
Train all staff/researchers embedded in services.
5. Exchange knowledge
Patient and public involvement-informed stakeholder knowledge exchange events.
Please see our participant recruitment details here















